Peripheral vascular disease- PAD
What Is It?
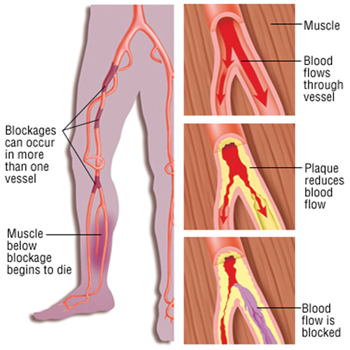
In peripheral arterial disease (previously called peripheral vascular disease), not enough blood flows to the legs. The condition usually is caused by fatty deposits called plaques that build up along the walls of blood vessels. This buildup shrinks the size of the passageway and reduces the amount of blood that can flow through. This is a condition called atherosclerosis.
Risk factors for getting peripheral arterial disease are similar to the risk factors for coronary heart disease, and include:
- Smoking cigarettes or using other forms of tobacco (such as snuff and chew)
- An abnormally high level of cholesterol (hypercholesterolemia)
- An abnormally low level of high-density lipoprotein (HDL, the good cholesterol)
- High blood pressure (hypertension)
- Diabetes
- Family history of cardiovascular disease
- Obesity
- Family history of cardiovascular disease
- Obesity
- Physical inactivity (too little regular exercise)
- Kidney disease
- Race (blacks appear to have a higher risk of developing the disease)
Symptoms
The most common symptom of peripheral arterial disease is intermittent claudication – pain or cramping in the legs or buttocks that starts when you exercise and goes away when you rest. Often the pain is described as a deep ache, especially in the calf muscle. The pain may extend to the foot or up toward the thigh and buttock. Sometimes, there is just numbness in the leg or a sense that one leg gets tired when you walk. A foot or toes also may feel cold or numb.
If the arteries are severely narrowed, you could experience leg pain at rest, when you are not exercising. If blood flow stops completely (usually because a blood clot forms in the narrowed vessel), parts of the leg may become pale or turn blue, feel stone cold to the touch and eventually develop gangrene.
Diagnosis
Techniques used to diagnose PVD include a medical history, physical examination, doppler ultrasound, computerized tomographic angiography (CTA) and magnetic resonance arteriography (MRA).
Probably the most useful, although underutilized, diagnostic tool for detecting peripheral arterial disease in the outpatient setting is the Ankle Brachial Index or ABI test. This simple, painless test compares the blood pressure in the legs to the blood pressure in the arms to help accurately measure the degree of blood flow in the lower extremities.
Underdiagnosed and undertreated
In contrast to coronary and cerebral artery disease, PVD is vastly underdiagnosed despite its abysmal mortality rates. it is estimated that less than 30% of PVD patients are diagnosed, mainly due to the fact that over 50% are asymptomatic – leg pain may be present in only 10% of patients.Lack of awareness and appreciation of PVD is a major contributing factor to the underdiagnosis of this serious disease.
Prevention
You can help to prevent peripheral arterial disease by modifying your risk factors:
Don’t smoke
This a major risk factor that you can control
Maintain a healthy weight
Obesity, especially a concentration of body fat around the waist, has been linked to unhealthy blood levels of cholesterol and other fats, which can build up inside your arteries.
Eat a healthy diet
Your diet should be loaded with vegetables and fruits, and it should be low in saturated fats
Exercise regularly
Ideally, you should exercise 45 minutes or more every day
Lower your blood pressure
Medications may be necessary if maintaining a healthy lifestyle is not enough
Treatment
- Modifying risk factors: Quitting smoking can reduce the symptoms of intermittent claudication
- Exercise programmes
- Medications
- Revascularization procedures: The goal of revascularization is to improve circulation, either by opening narrowed arteries or by bypassing the narrowed section of the artery. These procedures include surgical and non-surgical techniques and are used in people who have severe or progressive symptoms, or whose leg pain occurs at rest. The most common non-surgical procedure is percutaneous transluminal angioplasty, also called balloon angioplasty. In this procedure, a catheter is inserted into the narrowed artery and a small balloon at the tip is inflated to open the narrowed vessel. Often, a metallic implant called a stent is used as a scaffold to support the wall of the artery after it is opened with the balloon. In some people, the narrowed vessel must be bypassed surgically using either a section of vein taken from the leg or a synthetic graft.
When To Call a Professional
Call your doctor if you consistently suffer from cramps, aching, numbness or disproportionate fatigue in your leg muscles or buttocks when you exercise. Call immediately if you have these symptoms at rest or when any part of your leg or foot suddenly turns numb, cold, pale or a bluish color.
